Rethink Health: Inflammation Is Actually Repair Deficit: Using Physiology First to Achieve Better Outcomes Part 1: Value and Importance of Understanding Inflammation As Repair Deficit Opportunity
by Russell Jaffe, MD, PhD, CCN, and Jayashree Mani, MS, CCN
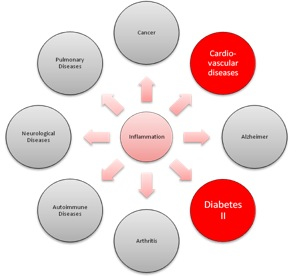
Inflammation is increasingly recognized as a cause or amplifier of all chronic, degenerative, and autoimmune conditions; the health challenges that rob many of their vitality and life quality (Figure 1). The many expressions of inflammation bring over 100,000 excess deaths adding an annual incremental health-care cost exceeding $200 billion. Lives and resources saved by correcting repair deficits can be repurposed to deliver higher-quality life for these people, their families, and communities, and at substantially lower net cost of health care because they have shifted from very high risk and cost to equally low risk and cost by choice and due to incentives for more healthful habits of daily living.
Figure 1: Inflammation
Part 1 of this article rethinks inflammation based on physiology rather than pathology and systems biology rather than mechanical engineering, finding insights and opportunities to improve outcomes at lower risks and costs.
Inflammation is revealed to be repair deficit and chronic inflammation is cumulative repair deficit. Inflammation has long been taught as a "fire" to be "fought" or a symptom to be suppressed. In contrast, repair deficits are opportunities to rebuild, renew, and rehabilitate as well as to remove obstacles to recovery by providing adequate amounts of essential health factors according to each individual's requirements.
This article explores inflammation's causes and consequences as cumulative repair deficits. Essential nutrient deficits, toxin excess, physical deconditioning and mental anguish potentiate and/or cause the blocks to recovery experienced and observed clinically as inflammation.
The immune defense and repair system's critical roles in inflammation are discussed here. A brief review of immune system functions is followed by a proven comprehensive integrative approach known as the Alkaline Way that engages the choices which people make about what they eat, drink, think, and do to evoke or inhibit healing responses. A goal is to meet individual needs so that repair can be completed and inflammation resolved naturally yet promptly and fully.
The Alkaline Way is an evidence-based personalized approach to redress the causes of inflammation and thus restore healthful resilience through enhanced enabled repair. The Alkaline Way concept has been successfully tested in controlled, community-based outcome studies of people with fibromyalgia, chronic fatigue syndrome, and both types of diabetes.1-3 Clinical reports from over 60,000 cases over 30 years indicate that all autoimmune conditions have mechanisms in common and clinically respond to this fundamental yet elegantly frugal approach. Small changes in what we eat, drink, think, and do can reward us with years or decades of quality life documented by independent predictive biomarkers. Choices of what we eat, drink, think and do determine 92% of our quality of life years (QoLY) that is epigenetic (RNAs) with 8% determined by genetics (DNA).
The Alkaline Way approach to personalized care includes identifying and substituting each of the individual's sources of foreign invaders known generally as antigens that can wear down the immune defense and repair system. Maldigestion and dietary intolerances as well as detoxification and neurohormonal balance are other aspects included in this approach to removing obstacles to recovery.4
The Alkaline Way includes a health-promoting, nutrient-dense, whole food, and fiber-rich diet; an active lifestyle; and targeted supplementation based on meeting individual needs, meaningful work, and nurturing relationships.5 The program is often more effective and brings more prompt and substantial relief than current best standard of allopathic care for that condition.
Inflammation Unmasked
In Western allopathic medicine, inflammation is seen as being either acute or chronic. In other healing arts, more nuanced approaches are taken to understanding the continuum of effective and ineffective repair systems, elective protective systems, and proactive health-promotion systems.
In Western allopathic medicine, inflammation is seen as being either acute or chronic. In other healing arts, more nuanced approaches are taken to understanding the continuum of effective and ineffective repair systems, elective protective systems, and proactive health-promotion systems.
Acute Inflammation
Acute inflammation is the short-term immune response that the body mounts in cases of trauma, infection, and allergy. Symptoms occur only when the immune defense and repair system uses up and runs out of essential protective, energizing nutrients and calls for help by recruiting additional aspects of the immune system.
Western medicine first recognized the four signs of inflammation 2000 years ago as tumor, rubor, calor and dolor, Latin for "swelling," "redness," "heat," and "pain." Galen, the Alexandrian physician redactor, a few hundred years later added functio laesa, Latin for "loss of function," as the fifth aspect or consequence of inflammation. Little has been done since until recent evidence revealed the upstream causes of downstream inflammation.
Besides physical changes, important psychological correlates may include lethargy, apathy, loss of appetite and increasing sensitivity to pain – a suite of symptoms that are collectively known as "sickness behavior."6 This article recommends using predictive biomarker tests to appreciate areas of strength and resilience while identifying areas in need of improving. The Alkaline Way of sustainable living includes measured, and effective means based on the aggregate evidence and experience.4
Acute inflammation is the short-term immune response that the body mounts in cases of trauma, infection, and allergy. Symptoms occur only when the immune defense and repair system uses up and runs out of essential protective, energizing nutrients and calls for help by recruiting additional aspects of the immune system.
Western medicine first recognized the four signs of inflammation 2000 years ago as tumor, rubor, calor and dolor, Latin for "swelling," "redness," "heat," and "pain." Galen, the Alexandrian physician redactor, a few hundred years later added functio laesa, Latin for "loss of function," as the fifth aspect or consequence of inflammation. Little has been done since until recent evidence revealed the upstream causes of downstream inflammation.
Besides physical changes, important psychological correlates may include lethargy, apathy, loss of appetite and increasing sensitivity to pain – a suite of symptoms that are collectively known as "sickness behavior."6 This article recommends using predictive biomarker tests to appreciate areas of strength and resilience while identifying areas in need of improving. The Alkaline Way of sustainable living includes measured, and effective means based on the aggregate evidence and experience.4
Chronic Inflammation
Chronic inflammation occurs when repair deficits persist. The body calls for repair, and the first-responder cell team is unable to complete the repair or defense mission. Recruits are called by pro-inflammatory signals. Pathology and conventional medicine sees inflammation as a persisting slow-burning fire, continuing to call for pro-inflammatory responses even as the immune systems are unable to meet the needed repair requirements because some essential factors are missing or from toxin exposures.
Physiology recognizes that persisting inflammation means accumulating repair deficits throughout the body, leading to many common chronic conditions. For example, persisting repair deficit in blood vessel linings can lead to atherosclerosis, coronary artery, and peripheral artery vascular diseases. In the endocrine organs such as the pancreas, thyroid or adrenal glands, (pathologies such as Cushing's hyperadrenalism or Addison's hypoadrenalism can occur.
Most chronic pain such as arthritis, bursitis, back pain, and costochondritis is a result of persisting repair deficit in joint tissue. If repair deficits persist in the gut lining, then loss of elective protective mechanism occurs. Lactose and gluten intolerance, as well as low mucosal antibody (IgA) and inflammatory bowel diseases, occur secondary to maldigestion, dysbiosis, and impaired repair of the gut resulting in compromised digestion, assimilation, and elimination.
Figure 1 shows how common and pervasive chronic inflammatory conditions are. Symptoms that people commonly associate with persisting chronic inflammation include body aches and pains, congestion, recurrent infections, diarrhea, dry eyes, indigestion, maldigestion, shortness of breath, skin outbreaks, swelling, stiffness, and weight gain/obesity.
Most pain medications work by blocking the repair process so that swelling reduces and pain abates. Blocking repair sets up a cycle of increasing inflammation that requires increasingly intensive immune suppression. Recent evidence understood in biological rather than mechanistic terms suggested there is a better way to improve outcomes more safely and with substantially less risk, collateral damage, and cost.
Conditions of cumulative repair deficit reduce life quality and increase costs of care that currently is mostly palliative and symptom suppressive rather than identifying and correcting the deficits or toxins that prevent full and enduring repair.7
Chronic inflammation occurs when repair deficits persist. The body calls for repair, and the first-responder cell team is unable to complete the repair or defense mission. Recruits are called by pro-inflammatory signals. Pathology and conventional medicine sees inflammation as a persisting slow-burning fire, continuing to call for pro-inflammatory responses even as the immune systems are unable to meet the needed repair requirements because some essential factors are missing or from toxin exposures.
Physiology recognizes that persisting inflammation means accumulating repair deficits throughout the body, leading to many common chronic conditions. For example, persisting repair deficit in blood vessel linings can lead to atherosclerosis, coronary artery, and peripheral artery vascular diseases. In the endocrine organs such as the pancreas, thyroid or adrenal glands, (pathologies such as Cushing's hyperadrenalism or Addison's hypoadrenalism can occur.
Most chronic pain such as arthritis, bursitis, back pain, and costochondritis is a result of persisting repair deficit in joint tissue. If repair deficits persist in the gut lining, then loss of elective protective mechanism occurs. Lactose and gluten intolerance, as well as low mucosal antibody (IgA) and inflammatory bowel diseases, occur secondary to maldigestion, dysbiosis, and impaired repair of the gut resulting in compromised digestion, assimilation, and elimination.
Figure 1 shows how common and pervasive chronic inflammatory conditions are. Symptoms that people commonly associate with persisting chronic inflammation include body aches and pains, congestion, recurrent infections, diarrhea, dry eyes, indigestion, maldigestion, shortness of breath, skin outbreaks, swelling, stiffness, and weight gain/obesity.
Most pain medications work by blocking the repair process so that swelling reduces and pain abates. Blocking repair sets up a cycle of increasing inflammation that requires increasingly intensive immune suppression. Recent evidence understood in biological rather than mechanistic terms suggested there is a better way to improve outcomes more safely and with substantially less risk, collateral damage, and cost.
Conditions of cumulative repair deficit reduce life quality and increase costs of care that currently is mostly palliative and symptom suppressive rather than identifying and correcting the deficits or toxins that prevent full and enduring repair.7
Inflammation and the Immune System
The immune defense and repair system responses, including neurohormonal modulators, are keys to a deeper understanding of inflammation. Together they are the neuroimmunohormonal governing system of the animal body.
Animal immune systems have two parts known as innate/intrinsic and adaptive/acquired that will now be described functionally.
The immune defense and repair system responses, including neurohormonal modulators, are keys to a deeper understanding of inflammation. Together they are the neuroimmunohormonal governing system of the animal body.
Animal immune systems have two parts known as innate/intrinsic and adaptive/acquired that will now be described functionally.
Innate Immune System
The innate immune system develops during the neonatal period concurrently with the digestive system. First responder or phagocytic cells are part of the innate immune system. First responder cells include the surveillance cells that traffic throughout the body as well as specialized cells inside each differentiated organ system. Examples include blood polymorphonuclear leukocytes, monocytes, basophils, and eosinophils as well as tissue mast cells, macrophages, fibroblasts, Kupffer cells in the liver, sinusoidal cells in the spleen, astrocytes in the brain, and so on.
The innate immune system develops during the neonatal period concurrently with the digestive system. First responder or phagocytic cells are part of the innate immune system. First responder cells include the surveillance cells that traffic throughout the body as well as specialized cells inside each differentiated organ system. Examples include blood polymorphonuclear leukocytes, monocytes, basophils, and eosinophils as well as tissue mast cells, macrophages, fibroblasts, Kupffer cells in the liver, sinusoidal cells in the spleen, astrocytes in the brain, and so on.
Acquired Immune System
The acquired immune system is adaptive. This aspect of the immune system is called upon and learns what additional defense or repair is needed beyond what the innate immune system can accomplish. The adaptive immune system develops based on interaction with its environment when innate responses lack the capacity to complete the tasks of recycling that which is not self and is thus foreign to the body.
In other words, the more toxins, disease causing bugs, or allergens that we are exposed to and successfully fend off beyond what the innate immune system can neutralize and recycle, the more our acquired immune system grows in complexity. However, when we exceed immune defense and repair competences, chronic, degenerative, and autoimmune diseases then emerge. These conditions have become so common that it is hard to find an asymptomatic healthy population upon which to standardize lab tests.
The acquired immune system is adaptive. This aspect of the immune system is called upon and learns what additional defense or repair is needed beyond what the innate immune system can accomplish. The adaptive immune system develops based on interaction with its environment when innate responses lack the capacity to complete the tasks of recycling that which is not self and is thus foreign to the body.
In other words, the more toxins, disease causing bugs, or allergens that we are exposed to and successfully fend off beyond what the innate immune system can neutralize and recycle, the more our acquired immune system grows in complexity. However, when we exceed immune defense and repair competences, chronic, degenerative, and autoimmune diseases then emerge. These conditions have become so common that it is hard to find an asymptomatic healthy population upon which to standardize lab tests.
Impact of a Burdened Immune System
Chronic infections, a telltale sign of a burdened immune system, also include inflammation repair deficits while also increasing the probability of concurrent metabolic imbalance, weight management issues, and insulin resistance leading to the continuum of prediabetes, diabetes, and the myriad heart and blood vessel consequences that ensue.
Additionally, inflammation usually so imbalances immune responses that delayed allergies develop because underlying maldigestion increases digestive remnants recognized as foreign by the body and not trapped by elective protective mechanisms such as mucins, sIgA, insoluble dietary fiber, and digestive enzymes. We find that delayed or late-phase food and other chemical sensitivities contribute in most people to chronic low-grade systemic inflammation and play a role in causing or amplifying autoimmune, chronic, and degenerative illnesses.
Perhaps one of the most baffling conditions of our times is cancer. In addition to chronic repair deferral, the repair system also eliminates the cancer cells that people form every day. One of the reasons for increased cancer risk is an immune system preoccupied with defense and unable to identify and eliminate the abnormal cells that form daily in all people.
Items taken up into the body are either nonthreatening and helpful or threatening and unhelpful. Infectious agents and digestive remnants (incompletely digested material) are treated equally by the immune system – both are considered foreign; that is, not "self tolerant."
Since defense takes precedence over repair in the immune system, digestive remnants occur due to maldigestion, prolonged transit time, and consequent toxicant reabsorption. Intestinal permeability increases due to cumulative repair deficits. Increased permeability allows digestive remnants to invade the body, increasing the defense work in the immune system. In chronic illness, underlying maldigestion and repair deficit set the stage for host hospitality to chronic infection and/or autoimmune, self-attacking chronic degenerative illnesses.
In healthy people pro-inflammatory compounds are released when needed and then turned off with anti-inflammatory antioxidants when the threat has been neutralized or the repair completed. Homeostasis or self reequilibration can thus be restored.
Chronic infections, a telltale sign of a burdened immune system, also include inflammation repair deficits while also increasing the probability of concurrent metabolic imbalance, weight management issues, and insulin resistance leading to the continuum of prediabetes, diabetes, and the myriad heart and blood vessel consequences that ensue.
Additionally, inflammation usually so imbalances immune responses that delayed allergies develop because underlying maldigestion increases digestive remnants recognized as foreign by the body and not trapped by elective protective mechanisms such as mucins, sIgA, insoluble dietary fiber, and digestive enzymes. We find that delayed or late-phase food and other chemical sensitivities contribute in most people to chronic low-grade systemic inflammation and play a role in causing or amplifying autoimmune, chronic, and degenerative illnesses.
Perhaps one of the most baffling conditions of our times is cancer. In addition to chronic repair deferral, the repair system also eliminates the cancer cells that people form every day. One of the reasons for increased cancer risk is an immune system preoccupied with defense and unable to identify and eliminate the abnormal cells that form daily in all people.
Items taken up into the body are either nonthreatening and helpful or threatening and unhelpful. Infectious agents and digestive remnants (incompletely digested material) are treated equally by the immune system – both are considered foreign; that is, not "self tolerant."
Since defense takes precedence over repair in the immune system, digestive remnants occur due to maldigestion, prolonged transit time, and consequent toxicant reabsorption. Intestinal permeability increases due to cumulative repair deficits. Increased permeability allows digestive remnants to invade the body, increasing the defense work in the immune system. In chronic illness, underlying maldigestion and repair deficit set the stage for host hospitality to chronic infection and/or autoimmune, self-attacking chronic degenerative illnesses.
In healthy people pro-inflammatory compounds are released when needed and then turned off with anti-inflammatory antioxidants when the threat has been neutralized or the repair completed. Homeostasis or self reequilibration can thus be restored.
An Integrative Approach to Restore and Repair
Better clinical outcomes incorporate new insights from molecular biology. The Alkaline Way of living is the clinical program or plan that best concurrently enables healthy immune, neurohormone, digestive, and detoxification system functions. The Alkaline Way includes the following four interdependent elements:
Better clinical outcomes incorporate new insights from molecular biology. The Alkaline Way of living is the clinical program or plan that best concurrently enables healthy immune, neurohormone, digestive, and detoxification system functions. The Alkaline Way includes the following four interdependent elements:
1. Functional Tests
Functional lab tests are suggested that are primary and predictive. Measures of energy metabolism, inflammation, detoxification, oxidative stress, metabolic status, cell communication, acid/alkaline balance, and immune system function are included because they are interdependent. Functional and predictive measures of loss of tolerance to food and environmental chemicals can now be determined by lymphocyte response assays (LRA by ELISA/ACT) that are among the breakthroughs included in this personalized approach to risk reduction.
Functional lab tests are suggested that are primary and predictive. Measures of energy metabolism, inflammation, detoxification, oxidative stress, metabolic status, cell communication, acid/alkaline balance, and immune system function are included because they are interdependent. Functional and predictive measures of loss of tolerance to food and environmental chemicals can now be determined by lymphocyte response assays (LRA by ELISA/ACT) that are among the breakthroughs included in this personalized approach to risk reduction.
2. Healthful Eating and Drinking
An alkalinizing eating plan establishes repair by maintaining healthy cell and body pH levels. There is aFood Effects on Body Chemistry chart that guides more healthful consumption. The Joy of Eating the Alkaline Way is available as a free downloadable summary or a purchasable e-book that includes details of speeding a tasty transition from foods that wear you out to foods that sustain and restore. High-fiber, healthier digestive transit time, enhanced detoxification, improved intestinal repair and function, and increased intake of essential nutrients are all woven into this approach.
An alkalinizing eating plan establishes repair by maintaining healthy cell and body pH levels. There is aFood Effects on Body Chemistry chart that guides more healthful consumption. The Joy of Eating the Alkaline Way is available as a free downloadable summary or a purchasable e-book that includes details of speeding a tasty transition from foods that wear you out to foods that sustain and restore. High-fiber, healthier digestive transit time, enhanced detoxification, improved intestinal repair and function, and increased intake of essential nutrients are all woven into this approach.
3. Supplementation
Individualized supplement protocols or flow charts address inflammation starting with specific nutrient deficits to make sure that the essentials that cannot be made are present in the amounts needed and in the right places for each individual. The level of toxins in the environment, the reduction in nutrient density in what most people eat, the intensity of distress, sedentary lifestyle – all add up to supplementation, often intensive supplementation, until repair deficit inflammation has been resolved.
Essential and conditionally essential nutrients are required to maintain or restore health rather than elective. Fortunately, using the predictive biomarker tests below, we can now personalize the nutrients needed, confirm the level of risk reduction through repeat tests, and confirm to individuals how much healthier they are on supplements that are needed for sustained health or to restore health.
Individualized supplement protocols or flow charts address inflammation starting with specific nutrient deficits to make sure that the essentials that cannot be made are present in the amounts needed and in the right places for each individual. The level of toxins in the environment, the reduction in nutrient density in what most people eat, the intensity of distress, sedentary lifestyle – all add up to supplementation, often intensive supplementation, until repair deficit inflammation has been resolved.
Essential and conditionally essential nutrients are required to maintain or restore health rather than elective. Fortunately, using the predictive biomarker tests below, we can now personalize the nutrients needed, confirm the level of risk reduction through repeat tests, and confirm to individuals how much healthier they are on supplements that are needed for sustained health or to restore health.
4. Healthy Thinking and Doing
Lifestyle choices with an emphasis on activity and mindfulness are geared towards enabling healing responses. Sitting for more than 20 minutes at a time turns out to be among the least healthful activities, particularly for digestion, circulation, and joint health. We suggest a timer that alerts the individual every 20 minutes to get up, stretch, look outside, or at least imagine that you are looking outside and appreciate whatever you have just accomplished or are making progress toward. A few deep abdominal breaths and whatever general and gentle stretching feels best. In addition, 20 minutes twice a day of mindfulness practice to cultivate awareness and nonattachment is an investment in long-term healthy equanimity.
Each step of this approach is described in greater detail below starting with the independent predictive biomarkers that allow each person to know status of key control systems in the body so that you can determine if you are getting all that your body needs to keep you as healthy as possible.
Lifestyle choices with an emphasis on activity and mindfulness are geared towards enabling healing responses. Sitting for more than 20 minutes at a time turns out to be among the least healthful activities, particularly for digestion, circulation, and joint health. We suggest a timer that alerts the individual every 20 minutes to get up, stretch, look outside, or at least imagine that you are looking outside and appreciate whatever you have just accomplished or are making progress toward. A few deep abdominal breaths and whatever general and gentle stretching feels best. In addition, 20 minutes twice a day of mindfulness practice to cultivate awareness and nonattachment is an investment in long-term healthy equanimity.
Each step of this approach is described in greater detail below starting with the independent predictive biomarkers that allow each person to know status of key control systems in the body so that you can determine if you are getting all that your body needs to keep you as healthy as possible.
Functional Tests: Predictive Biomarkers
The following functional markers are predictive of outcome and useful in monitoring therapeutic outcomes and responses. These tests have been chosen because taken together they cover the major aspects of metabolism. In addition, these tests have been done on large enough populations and with long enough follow-up that results from these predictive biomarker tests can be translated into years or decades of life at risk, retainable, or reserved depending on the individual's tests results. In addition, we suggest interpreting each individual's tests results compared with the best outcome value for the biomarker. The seven tests that follow have been selected as most predictive and most actionable if test results are not at their goal or best outcome value:
The following functional markers are predictive of outcome and useful in monitoring therapeutic outcomes and responses. These tests have been chosen because taken together they cover the major aspects of metabolism. In addition, these tests have been done on large enough populations and with long enough follow-up that results from these predictive biomarker tests can be translated into years or decades of life at risk, retainable, or reserved depending on the individual's tests results. In addition, we suggest interpreting each individual's tests results compared with the best outcome value for the biomarker. The seven tests that follow have been selected as most predictive and most actionable if test results are not at their goal or best outcome value:
- Sugar, energy, metabolism: Hgb A1c, fuctosamine, glycation products tests
- Inflammation: hsCRP, sedimentation rate (sed rate), fibrinogen, ferritin, tumor necrosis factor (TNF), certain cytokines and microalbumin, among other inducible proteins
- Detoxification and methylation status: Homocysteine
- Oxidative stress, free radical activity and antioxidant status: Oxidized LDL/HDL & 8-oxo-guanine
- Metabolic status and acid/alkaline balance: 1st urine pH after 6+ hours rest
- Cell communication: 25-OH vitamin D
- Immune tolerance or reactivity: LRA by ELISA/ACT tests
While most labs report a usual or "normal" range for lab results, this information is of use for comparative, statistical but not predictive, clinical purposes. The test value can be used to calculate the years or decades of life either gained or lost, depending on the value for the test obtained for that individual. Predictive biomarker tests are referenced or interpreted based on goal value. For more details, visithttp://betterlabtestsnow.com/predictive-bio-markers-panel.aspx.
We find that use of goal values represents the best current predictors of health risk or resilience. These tests can be influenced by epigenetic lifestyle actions to influence all-cause morbidity and mortality. Predictive biomarker test results allow a comprehensive yet accessible, actionable personalized, comprehensive health plan. Best outcome goal values are also useful in comparative effectiveness research where objective discriminators are needed when comparing complex therapies in the community.
Best outcome or goal values (GV) follow:
We find that use of goal values represents the best current predictors of health risk or resilience. These tests can be influenced by epigenetic lifestyle actions to influence all-cause morbidity and mortality. Predictive biomarker test results allow a comprehensive yet accessible, actionable personalized, comprehensive health plan. Best outcome goal values are also useful in comparative effectiveness research where objective discriminators are needed when comparing complex therapies in the community.
Best outcome or goal values (GV) follow:
- Hgb A1c < 5 mg/dl
- hsCRP < 0.5 mg/L8
- homocysteine < 6 µmol/L9
- oxidized HDL/LDL10 and 8-oxo-guanine11 ~0
- 1st AM urine pH12 6.5–7.5
- Vitamin D13 (25-OH D) 50–80 ng/L
- LRA by ELISA/ACT tests; "healthy" means complete tolerance and no delayed allergies
Note that the healthy or goal values above are based on least risk rather than statistical calculations. This means that reported usual or normal ranges for the above tests on lab reports will be different. Usual or normal ranges tell little or nothing about individual relative risk. "Normal" or "usual" lab ranges are calculated and really only reveal if a person is sicker than the population used to standardize the test. Since ambulatory people not known to have the problem are used to establish reference "normal" or "usual" ranges, you only get statistical information. This is useful in distinguishing groups or populations. Unfortunately, since healthy, asymptomatic people are not used to standardize tests, all you really get is information compared to a population. Determining test sensitivity, specificity and predictive index were the best that could be done until functional or predictive tests became available.14
Predictive biomarker test values are consistent with the concept of "optimum" or "high level health" values championed by Cheraskin and Ringsdorf or the individual needs for nutrients pioneered by Roger Williams.15,16
Predictive biomarker test values are consistent with the concept of "optimum" or "high level health" values championed by Cheraskin and Ringsdorf or the individual needs for nutrients pioneered by Roger Williams.15,16
Testing Delayed Allergies: Functional LRA by ELISA/ACT Tests Is Predictive
Delayed allergies are another indicator of a burdened or imbalanced immune system that can contribute to many of the chronic and degenerative illnesses already discussed. Various clinical tests have been used to assess individual adverse responses to environmental antigens.17 Antibodies capable of inciting a delayed response include IgM, sIgA, IgA, and IgG as well as immune complexes and T cell reactions. Serology (antibody) tests are often misleading because they do not distinguish helpful from harmful antibodies. Functional tests such as lymphocyte response assays (LRAs) do not suffer from this methodological limitation.
Delayed allergies are another indicator of a burdened or imbalanced immune system that can contribute to many of the chronic and degenerative illnesses already discussed. Various clinical tests have been used to assess individual adverse responses to environmental antigens.17 Antibodies capable of inciting a delayed response include IgM, sIgA, IgA, and IgG as well as immune complexes and T cell reactions. Serology (antibody) tests are often misleading because they do not distinguish helpful from harmful antibodies. Functional tests such as lymphocyte response assays (LRAs) do not suffer from this methodological limitation.
Limitations of Common Delayed Allergy Tests
IgG antibody assays are performed to detect immunoglobulin G (IgG).18 This has the advantage of examining the system's immunologic memory. Note that most IgG antibodies are helpful, neutralizing, and protective. Only a minority of them are harmful, symptom provoking, and bad.19 Our estimate is that at least 80% of IgG antibodies are helpful and that less than 20% are harmful. More importantly, tests that do not distinguish helpful from harmful results are of limited predictive significance at best. IgG protective antibodies from childhood infections are helpful and not signs of "delayed allergy" to the infection.
IgG antibody assays are performed to detect immunoglobulin G (IgG).18 This has the advantage of examining the system's immunologic memory. Note that most IgG antibodies are helpful, neutralizing, and protective. Only a minority of them are harmful, symptom provoking, and bad.19 Our estimate is that at least 80% of IgG antibodies are helpful and that less than 20% are harmful. More importantly, tests that do not distinguish helpful from harmful results are of limited predictive significance at best. IgG protective antibodies from childhood infections are helpful and not signs of "delayed allergy" to the infection.
Four subclasses of IgG have been identified, which have different biologic functions and vary independently in different clinical conditions.20,21 Clinical interpretation of total IgG antibodies against a specific antigen can be a challenge.22 IgG1 is considered to be primarily for response to bacteria and accounts for 60% to 75% of all IgG. IgG2 is considered to be primarily for response to mucosal or respiratory infections and foreign antigens that access the same areas and accounts for 20% to 30% of all IgG. IgG3 is considered to be primarily for response to atypical substances and accounts for 5% to 8% of all IgG. IgG4 is usually the smallest fraction with the function of balancing specific IgE to reduce or prevent histaminic reactions including to parasites, accounting for just 1% to 4% of total IgG. Only IgG4 is cytophilic for mast cells.23 Thus, some IgG antibodies are protective and others harmful; quantitative serology tests do not distinguish between them.24
Quantitation of IgG antibodies omits information about IgA, sIgA, IgM, immune complex, and T cell offenders while needing multiple subclass assays to provide any predictive clinical information.25 In practice, IgG test results show high rates of false positive and false negative results. This hurts patient compliance and limits successful outcomes.
Immune complex or complement fixation tests can be done in a variety of ways, each with its own methodology limitations.26
Automated cytotoxic tests attempt to identify delayed allergies but only look at cell size change, giving the impression that lymphocytes are tested when any particle of a predetermined size is actually being measured. Understandably, these tests have low reproducibility and offer only short-term benefits.27
LRA Tests Are Functional, Predictive, and More Evidence Based
LRA by ELISA/ACT and MELISA tests both assess reactions of lymphocytes exposed in the lab to different substances but are different by design. Through the technology breakthrough involved in the LRA by ELISA/ACT methodology, it is possible to allow living white cells to react in the laboratory just as they do in the body.28 This determines true delayed allergy/hypersensitivity based on the body's long-lived memory-carrying white blood cells. LRA by ELISA/ACT tests are also unique in that all 3 delayed hypersensitivity pathways are measured on the same specimen and at the same time. The clinical results are more true positive and few false negative reactions confirmed in multiple successful community-based controlled outcome studies.29,30
The acute and delayed allergy pathways are depicted in the "Wheel of Immune Response Mechanism" (Figure 2).31
LRA by ELISA/ACT and MELISA tests both assess reactions of lymphocytes exposed in the lab to different substances but are different by design. Through the technology breakthrough involved in the LRA by ELISA/ACT methodology, it is possible to allow living white cells to react in the laboratory just as they do in the body.28 This determines true delayed allergy/hypersensitivity based on the body's long-lived memory-carrying white blood cells. LRA by ELISA/ACT tests are also unique in that all 3 delayed hypersensitivity pathways are measured on the same specimen and at the same time. The clinical results are more true positive and few false negative reactions confirmed in multiple successful community-based controlled outcome studies.29,30
The acute and delayed allergy pathways are depicted in the "Wheel of Immune Response Mechanism" (Figure 2).31
Figure 2
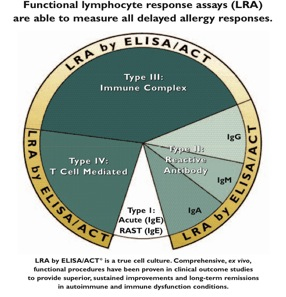
By testing lymphocyte reactions to purified antigens, it is possible to accurately assess the burden on immune defense and repair systems. The LRA by ELISA/ACT functional tests have a 97% accuracy rate substantially better than static, nonfunctional IgG testing and other automated cytotoxic, particle size procedures that give ambiguous results at best.32,33
The upstream causes of autoimmunity include acquired reactions to foods or other chemicals to which the body had become hypersensitive during times of distress, marked by enhanced antibody, immune complex, or T cell lymphocyte white cell responses that increase activity yet decrease functional benefits.
Part 1 of the this article has focused on the superior value of functional rather than static, conventional tests to guide advanced, personalized care. Predictive biomarker tests are suggested as an objective means of determining resilience or risk for each individual. Part 2 will present suggestions of what actions to take based on this evidence and synthesis for better outcomes with greater value and lower costs.
Resources
LRA by ELISA/ACT tests are available from:
ELISA/ACT Biotechnologies
109 Carpenter Dr., Suite 100
Sterling, Virginia 20164
800-553-5472
ClientServices@ELISAACT.com
www.ELISAACT.com
LRA by ELISA/ACT tests are available from:
ELISA/ACT Biotechnologies
109 Carpenter Dr., Suite 100
Sterling, Virginia 20164
800-553-5472
ClientServices@ELISAACT.com
www.ELISAACT.com
Nutritional supplements mentioned in this article are available from:
PERQUE Integrative Health
44621 Guilford Drive, Suite 150
Ashburn, Virginia 20147
800-525-7372
Clientservices2@PERQUE.com
www.PERQUE.com
PERQUE Integrative Health
44621 Guilford Drive, Suite 150
Ashburn, Virginia 20147
800-525-7372
Clientservices2@PERQUE.com
www.PERQUE.com
For functional biomarker tests:
Better Lab Tests Now
clientservices@BetterLabTestsNow.com
www.BetterLabTestsNow.com
http://betterlabtestsnow.com/predictive-bio-markers-panel.aspx
ZRT Lab
Doctor's Data, Inc.
Shiel Lab
Better Lab Tests Now
clientservices@BetterLabTestsNow.com
www.BetterLabTestsNow.com
http://betterlabtestsnow.com/predictive-bio-markers-panel.aspx
ZRT Lab
Doctor's Data, Inc.
Shiel Lab
Notes
1. Deuster PA, Jaffe R. A novel treatment for fibromyalgia improves clinical outcomes in a community based study. J Musculo Pain, 1998;6:133–149.
2. Jaffe R. First-line comprehensive care III: update on immune system lab tests for fibromyalgia-chronic fatigue-metabolic syndrome: continuum of treatment-resistant pain and fatigue: optimum clinical management improves outcomes and reduces risks and treatment complications as supported by new data. Townsend Lett. 2008;Jan:87–94.
3. Jaffe R, Mani J, DeVane J, Mani H. Tolerance loss in diabetics: association with foreign antigen exposure. Diabet Med. 2006;23(8):924–925.
4. Jaffe R. Quercetin & OPC: nature's solution to inflammation [webinar]. http://bit.ly/10z5ct6.
5. Health Studies Collegium. The Joy of Food: The Alkaline Way Guide. 18th ed. 1992–2010. www.HeatlhStudiesCollegium.org.
6. Holmes C, Cunningham C, Zotova E, Culliford D, Perry VH. Proinflammatory cytokines, sickness behavior, and Alzheimer disease. Neurology,2012;77(3):212–218.
7. Schmidt MI, Duncan BB. Diabesity: an inflammatory metabolic condition (review). Clin Chem Lab Med. 2003 Sep;41(9):1120–1130.
8. Ballantyne CM, Hoogeveen RC, Bang H, et al. Lipoprotein-associated phospholipase a2, high-sensitivity c-reactive protein, and risk for incident coronary heart disease in middle-aged men and women in the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2004;109:837–842 .
9. Nygård O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997 Jul 24;337(4):230–236.
10.Mertens A, Holvoet P. Oxidized LDL and HDL: antagonists in atherothrombosis. FASEB J.2001 Oct;15(12):2073–2084.
11.Markkanen E, Hübscher U, van Loon B. Regulation of oxidative DNA damage repair: The adenine:8-oxo-guanine problem. Cell Cycle. Epub 2012 Mar 15;11(6).
12.Hohenberger EF, Kimling H. Compendium urinalysis: urinalysis with test strips. 2002http://www.diavant.com/diavant/servlet/MDBOutput?fileId=1392.
13.Heaney RP. Vitamin D in health and disease. Clin J Am Soc Nephrol. 2008 Sep;3(5):1535–1541.
14.Galen RS, Gambino SR. Beyond Normality: The Predictive Value and Efficiency of Medical Diagnosis. New York: Wiley; 1975.
15.Cheraskin E, Ringsdorf WM Jr, Clark JW. Diet and Disease. Emmaus, PA: Rodale Books; 1968.
16.Williams RJ. Biochemical Individuality: The Key to Understanding What Shapes Your Health.New Canaan, CT: Keats Publishing; 1998.
17.Scadding GK, Brostoff J. Immunological response to food. In: Hunter JO, Jones VA, eds. Food and the Gut. Sussex, UK: Saunders; 1985.
18.Walker WA. Mechanisms of antigen handling by the gut. In: Ballieux I, ed. Clinics in Immunology and Allergy. Sussex, UK: Saunders; 1982.
19.Kotler DP, Gaetz HP, Lange M. Enteropathy associated with the acquired immune deficiency syndrome. Ann Int Med. 1984;101:421–428.
20.Roitt I, Brostoff J, Male D. Immunology. 6th ed. St. Louis: Mosby; 1993.
21.Male D, Brostoff J, Roitt I, Roth DB. Immunology. 7th ed. Mosby Elsevier; 2006.
22.Crisp HC, Quinn JM. Quantitative immunoglobulins in adulthood. Allergy Asthma Proc. 2009;30(6):649–654.
23. Lux A, Aschermann S, Biburger M, Nimmerjahn F. The pro and anti-inflammatory activities of immunoglobulin G. Ann Rheum Dis. 2010;69 Suppl 1:i92–96.
24. Woof JM, Mestecky J. Mucosal immunoglobulins – review. Immunol Rev. 2005:64–82.
25. Woof JM, Kerr MA. The function of immunoglobulin A in immunity. J Pathol. 2007;208(2):270–282.
26. Laevy O. Unmasking IgG responses. Nat Rev Immunol. 2006;6:632.
27. Hodsdon, W., Zwickey, H. Reproducibility and reliability of two food allergy testing methods. Nat Med J. 2010;2(3):8–13.
28. Jaffe R. Improved immune function using specific nutrient supplementation and ELISA/ACT "immunologic fingerprint" to detect late phase responses ex vivo. J Am Coll Nutr.1989;8(5):424.
29.Deuster PA, Jaffe R. A novel treatment for fibromyalgia improves clinical outcomes in a community based study. J Musculo Pain. 1998;6:133–149; Jaffe R, Mani J, DeVane J, Mani H. Tolerance loss in diabetics: Association with foreign antigen exposure. Diabet Med. 2006;23(8):924–925.
30.ELISA/ACT Biotechnologies Newsletter. 2010;1(2). Available at www.ELISAACT.com.
31.Jaffe R. Functional lab tests to evaluate immune competencies in chronic illness and chronic infection.Townsend Lett. 2009;306:80–90.
32.Report on Quality Control and Reproducibility of LRA by ELISA/ACT Tests. HSC Report 022010.
33.Hodsdon W, Zwickey H. NMJ original research: reproducibility and reliability of two food allergy testing methods. Nat Med J. 2010;2(3):8–13.
1. Deuster PA, Jaffe R. A novel treatment for fibromyalgia improves clinical outcomes in a community based study. J Musculo Pain, 1998;6:133–149.
2. Jaffe R. First-line comprehensive care III: update on immune system lab tests for fibromyalgia-chronic fatigue-metabolic syndrome: continuum of treatment-resistant pain and fatigue: optimum clinical management improves outcomes and reduces risks and treatment complications as supported by new data. Townsend Lett. 2008;Jan:87–94.
3. Jaffe R, Mani J, DeVane J, Mani H. Tolerance loss in diabetics: association with foreign antigen exposure. Diabet Med. 2006;23(8):924–925.
4. Jaffe R. Quercetin & OPC: nature's solution to inflammation [webinar]. http://bit.ly/10z5ct6.
5. Health Studies Collegium. The Joy of Food: The Alkaline Way Guide. 18th ed. 1992–2010. www.HeatlhStudiesCollegium.org.
6. Holmes C, Cunningham C, Zotova E, Culliford D, Perry VH. Proinflammatory cytokines, sickness behavior, and Alzheimer disease. Neurology,2012;77(3):212–218.
7. Schmidt MI, Duncan BB. Diabesity: an inflammatory metabolic condition (review). Clin Chem Lab Med. 2003 Sep;41(9):1120–1130.
8. Ballantyne CM, Hoogeveen RC, Bang H, et al. Lipoprotein-associated phospholipase a2, high-sensitivity c-reactive protein, and risk for incident coronary heart disease in middle-aged men and women in the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2004;109:837–842 .
9. Nygård O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997 Jul 24;337(4):230–236.
10.Mertens A, Holvoet P. Oxidized LDL and HDL: antagonists in atherothrombosis. FASEB J.2001 Oct;15(12):2073–2084.
11.Markkanen E, Hübscher U, van Loon B. Regulation of oxidative DNA damage repair: The adenine:8-oxo-guanine problem. Cell Cycle. Epub 2012 Mar 15;11(6).
12.Hohenberger EF, Kimling H. Compendium urinalysis: urinalysis with test strips. 2002http://www.diavant.com/diavant/servlet/MDBOutput?fileId=1392.
13.Heaney RP. Vitamin D in health and disease. Clin J Am Soc Nephrol. 2008 Sep;3(5):1535–1541.
14.Galen RS, Gambino SR. Beyond Normality: The Predictive Value and Efficiency of Medical Diagnosis. New York: Wiley; 1975.
15.Cheraskin E, Ringsdorf WM Jr, Clark JW. Diet and Disease. Emmaus, PA: Rodale Books; 1968.
16.Williams RJ. Biochemical Individuality: The Key to Understanding What Shapes Your Health.New Canaan, CT: Keats Publishing; 1998.
17.Scadding GK, Brostoff J. Immunological response to food. In: Hunter JO, Jones VA, eds. Food and the Gut. Sussex, UK: Saunders; 1985.
18.Walker WA. Mechanisms of antigen handling by the gut. In: Ballieux I, ed. Clinics in Immunology and Allergy. Sussex, UK: Saunders; 1982.
19.Kotler DP, Gaetz HP, Lange M. Enteropathy associated with the acquired immune deficiency syndrome. Ann Int Med. 1984;101:421–428.
20.Roitt I, Brostoff J, Male D. Immunology. 6th ed. St. Louis: Mosby; 1993.
21.Male D, Brostoff J, Roitt I, Roth DB. Immunology. 7th ed. Mosby Elsevier; 2006.
22.Crisp HC, Quinn JM. Quantitative immunoglobulins in adulthood. Allergy Asthma Proc. 2009;30(6):649–654.
23. Lux A, Aschermann S, Biburger M, Nimmerjahn F. The pro and anti-inflammatory activities of immunoglobulin G. Ann Rheum Dis. 2010;69 Suppl 1:i92–96.
24. Woof JM, Mestecky J. Mucosal immunoglobulins – review. Immunol Rev. 2005:64–82.
25. Woof JM, Kerr MA. The function of immunoglobulin A in immunity. J Pathol. 2007;208(2):270–282.
26. Laevy O. Unmasking IgG responses. Nat Rev Immunol. 2006;6:632.
27. Hodsdon, W., Zwickey, H. Reproducibility and reliability of two food allergy testing methods. Nat Med J. 2010;2(3):8–13.
28. Jaffe R. Improved immune function using specific nutrient supplementation and ELISA/ACT "immunologic fingerprint" to detect late phase responses ex vivo. J Am Coll Nutr.1989;8(5):424.
29.Deuster PA, Jaffe R. A novel treatment for fibromyalgia improves clinical outcomes in a community based study. J Musculo Pain. 1998;6:133–149; Jaffe R, Mani J, DeVane J, Mani H. Tolerance loss in diabetics: Association with foreign antigen exposure. Diabet Med. 2006;23(8):924–925.
30.ELISA/ACT Biotechnologies Newsletter. 2010;1(2). Available at www.ELISAACT.com.
31.Jaffe R. Functional lab tests to evaluate immune competencies in chronic illness and chronic infection.Townsend Lett. 2009;306:80–90.
32.Report on Quality Control and Reproducibility of LRA by ELISA/ACT Tests. HSC Report 022010.
33.Hodsdon W, Zwickey H. NMJ original research: reproducibility and reliability of two food allergy testing methods. Nat Med J. 2010;2(3):8–13.
 Dr. Russell Jaffe received his AB, MD (with senior thesis honors), and PhD (In biochemistry and physiology) from Boston University. Dr. Jaffe served his medical internship at University Hospital and was awarded a the US Public Health Service Officer Commission, assigned to the Clinical Center of the National Institutes of Health, in June 1973. While at the Clinical Center, Dr. Jaffe served his residency in clinical pathology. He is board certified in clinical and subspecialty certified in chemical pathology. Dr. Jaffe remained on the permanent senior staff of the NIH Clinical Pathology Department, where he continued method innovation and was active in collaborative research with the Laboratory of Experimental Atherosclerosis (of the Heart, Lung, and Blood Institute). Concurrently, Dr. Jaffe's interests in the mechanisms of health and the evoking of human healing responses led him to apprentice in such healing arts as acupuncture; mindfulness; massage; music, art, and color therapy; and a variety of eclectic therapeutic approaches. In addition, Dr. Jaffe performed innovative studies of platelet function and blood clotting in relation to the origins of coronary artery and cardiovascular diseases. Among the tests that he developed are the early colon cancer-screening test using occult blood detection not interfered with by vitamin C consumption, as well as a variety of tests related to the blood clotting and immune defense and repair systems. Dr. Jaffe developed the first method of measuring cell-mediated immunity using a modified ELISA system in a lymphocyte mitogenesis/blastogenesis brief cell culture known as lymphocyte response assays (LRA). This LRA by ELISA/ACT provides an "immunologic fingerprint" of items to which the body is reactive or tolerant. Dr. Jaffe has contributed over 100 symposium-invited talks, scientific articles, or book chapters. He received the J. D. Lane award for original research from the USPHS, the Merck Sharp and Dohme Excellence in Research Award, and in 2002 the International Research Scientist of the Year, among other recognitions for his investigations. Dr. Jaffe is a fellow of the Health Studies Collegium and director of ELISA/ACT Biotechnologies LLC and PERQUE LLC in Ashburn, Virginia. He may be reached at 800-525-7372 ext. 5101, and rjaffe@ELISAACT.com or rjaffe@PERQUE.com.
Dr. Russell Jaffe received his AB, MD (with senior thesis honors), and PhD (In biochemistry and physiology) from Boston University. Dr. Jaffe served his medical internship at University Hospital and was awarded a the US Public Health Service Officer Commission, assigned to the Clinical Center of the National Institutes of Health, in June 1973. While at the Clinical Center, Dr. Jaffe served his residency in clinical pathology. He is board certified in clinical and subspecialty certified in chemical pathology. Dr. Jaffe remained on the permanent senior staff of the NIH Clinical Pathology Department, where he continued method innovation and was active in collaborative research with the Laboratory of Experimental Atherosclerosis (of the Heart, Lung, and Blood Institute). Concurrently, Dr. Jaffe's interests in the mechanisms of health and the evoking of human healing responses led him to apprentice in such healing arts as acupuncture; mindfulness; massage; music, art, and color therapy; and a variety of eclectic therapeutic approaches. In addition, Dr. Jaffe performed innovative studies of platelet function and blood clotting in relation to the origins of coronary artery and cardiovascular diseases. Among the tests that he developed are the early colon cancer-screening test using occult blood detection not interfered with by vitamin C consumption, as well as a variety of tests related to the blood clotting and immune defense and repair systems. Dr. Jaffe developed the first method of measuring cell-mediated immunity using a modified ELISA system in a lymphocyte mitogenesis/blastogenesis brief cell culture known as lymphocyte response assays (LRA). This LRA by ELISA/ACT provides an "immunologic fingerprint" of items to which the body is reactive or tolerant. Dr. Jaffe has contributed over 100 symposium-invited talks, scientific articles, or book chapters. He received the J. D. Lane award for original research from the USPHS, the Merck Sharp and Dohme Excellence in Research Award, and in 2002 the International Research Scientist of the Year, among other recognitions for his investigations. Dr. Jaffe is a fellow of the Health Studies Collegium and director of ELISA/ACT Biotechnologies LLC and PERQUE LLC in Ashburn, Virginia. He may be reached at 800-525-7372 ext. 5101, and rjaffe@ELISAACT.com or rjaffe@PERQUE.com. Jayashree Mani, MS, CCN is a clinical nutritionist with over 20 years' experience in providing nutritional counseling and education to patients and physicians in various medical environments. Her focus over the past 10 years has been on the functional use of lymphocyte cell response assays in clinical management of various autoimmune conditions, including fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome. Developing nutritional protocols involving the Alkaline Way and specific nutritional supplementation, her work also includes specific emphasis on diabetes and metabolic syndrome and its management. She has coauthored chapters on these topics and published scientific articles describing these comprehensive approaches as well. She may be contacted at PERQUE Integrative Health/ELISA/ACT Biotechnologies; 800-525-7372 or 703-840-4427; jmani@PERQUE.com or jmani@elisaact.com.
Jayashree Mani, MS, CCN is a clinical nutritionist with over 20 years' experience in providing nutritional counseling and education to patients and physicians in various medical environments. Her focus over the past 10 years has been on the functional use of lymphocyte cell response assays in clinical management of various autoimmune conditions, including fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome. Developing nutritional protocols involving the Alkaline Way and specific nutritional supplementation, her work also includes specific emphasis on diabetes and metabolic syndrome and its management. She has coauthored chapters on these topics and published scientific articles describing these comprehensive approaches as well. She may be contacted at PERQUE Integrative Health/ELISA/ACT Biotechnologies; 800-525-7372 or 703-840-4427; jmani@PERQUE.com or jmani@elisaact.com.
No comments:
Post a Comment